Intent To Harm
The new doctor in town was friendly, popular—and dangerous. Especially to the nurses who reported his bizarre treatments.
Before everything happened, nurse Anne Mitchell says Kermit had a good little hospital. “We had an excellent nursing staff. We had great doctors. We provided very, very good care.”
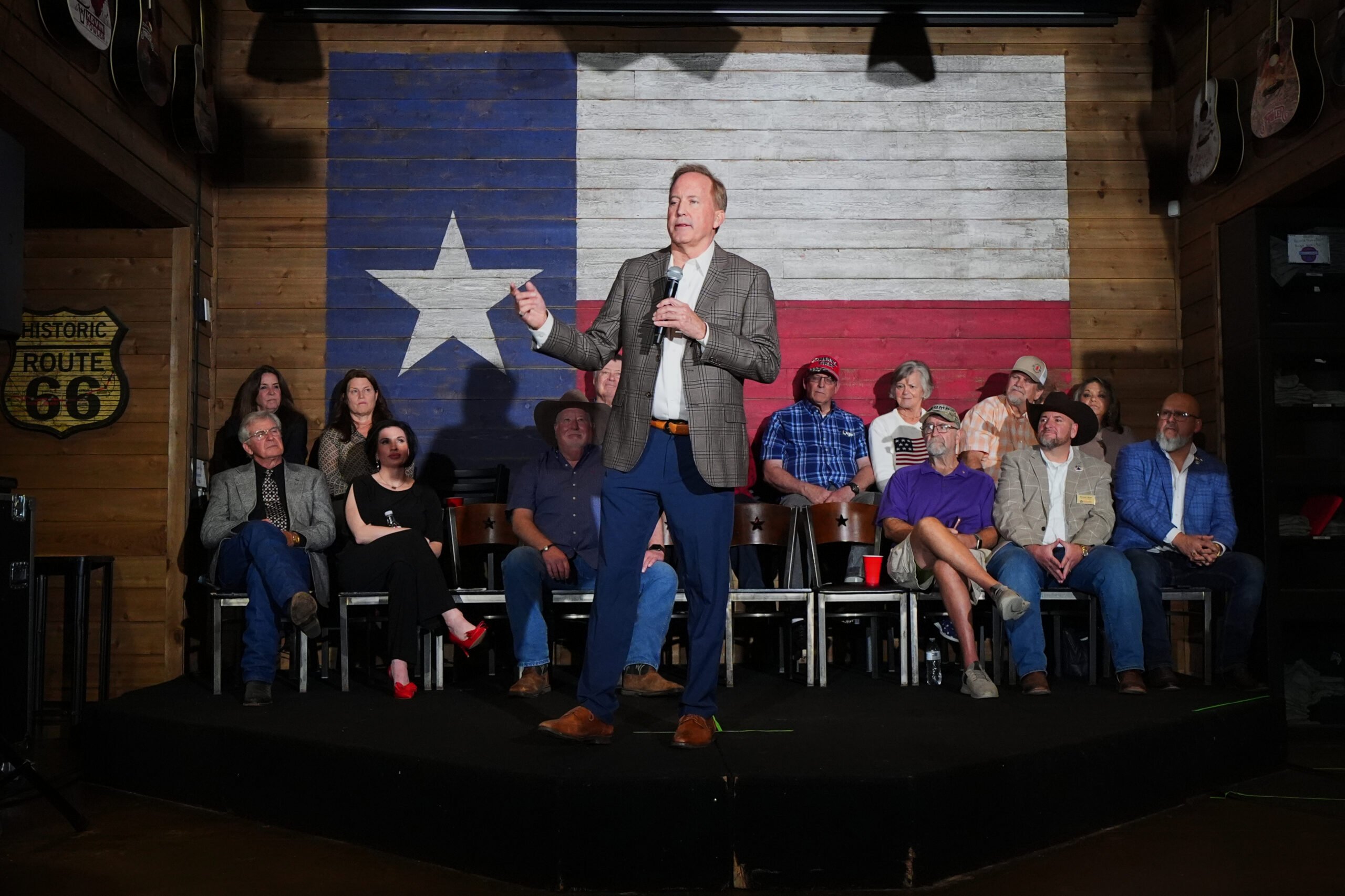
In 2008, when the trouble began, Winkler County Memorial Hospital was the pride of Kermit, one of the few new buildings and success stories in town. This flat, dusty burg of 5,000, 35 miles west of Odessa, is a ramshackle prairie town sprawling along Highway 18 in a motley collection of cinderblock and prefab siding. In the center of town, surrounded by a well-kept lawn and shuttered storefronts, sits a stately Depression-era courthouse. From any vantage point, you can see the face of Kermit the Frog, staring down at you from the water tower.
Before oil was discovered here in 1926, there was serious talk that the economic salvation of the county would be its sand, which residents hoped to sell in the Northeast for glassmaking. The oil boom altered that plan, catapulting a few local residents into staggering wealth. Those families—the Waltons, the Lecks, the Beckhams—still run things. The oil is still there, though the boom days are long over. On every road into town, pumps still peck at the ground, but fewer and fewer men work them. There is less and less work, period. Folks talk of the old days, when you didn’t have to drive to Odessa for everything.
If you get hurt in Kermit, as in most small Texas towns, there is one place to go. Car accidents, roughnecks with chemical burns, women in sudden labor—they all go to Winkler Memorial. It’s small, with 25 beds and two or three doctors on staff. But in the ultramodern, $13 million facility that opened in 2007 to replace the old hospital, Winkler Memorial provided basic care that a small community needs. Surgeries, non-emergency baby deliveries, serious trauma and other specialized procedures were sent to the bigger hospital in Odessa.
When the medical care is excellent, Kermit residents’ lack of choice isn’t a problem. But in a facility with just two or three doctors, it doesn’t take much to change the quality of care from excellent to downright dangerous. Until 2008, Winkler’s doctors were mostly foreigners, recent medical school graduates from places like India or Vietnam, here under the State Department’s J1 visa program. They usually worked three years, then moved on to bigger cities, bigger hospitals. Nurses were the backbone of Winkler Memorial, as they are at most small-town hospitals in Texas—experienced pros who could train the new doctors and monitor their work.
When the new hospital opened, Mitchell and fellow nurse Vickilyn Galle had been stalwarts of the Winkler Memorial staff for more than two decades. “I worked all over that hospital,” Mitchell says. “I was in infection control. I worked in home health. I was the director of nursing. I thought I’d work there till I retired.”
The two made an odd pair. Mitchell, a New York native, is serious and blunt. Galle, a native of nearby Jal, N.M., is quieter, grandmotherly; when Mitchell talks, Galle tends to fade into the background. But their approach to their work was the same. “The most important thing for us was the patients,” Mitchell says. “We were trained to look at every case and ask, how would I want a member of my family treated?”
In late 2007, when the hospital’s Board of Control replaced its retiring administrator, Galle was in charge of Winkler Memorial’s quality assessment program, which audited hospital records to monitor quality of care. Mitchell was the compliance officer, charged with making sure the hospital’s doctors and pharmacists stayed in line with state regulations. The hospital administration, they say, had always recognized the value of nurses’ role in overseeing the quality of care. “Everything was accessible,” Mitchell says. “There was nothing we couldn’t ask about or look at or have input into.” The budget was always tight, says another longtime nurse practitioner, Naomi Warren, but “we never compromised patient care.”
When the board hired Stan Wiley as the new administrator, that all changed. Wiley had left a job as hospital administrator in nearby Crane under cloudy circumstances. When he was hired at Winkler Memorial, he was selling mobile homes. Upon his arrival, Warren says Wiley made his priorities clear: He was going to bring in more revenue, and he was going to find doctors to move permanently to Kermit, ending the reliance on visa doctors.
Warren was skeptical. “It’s hard to get good doctors to move to a place like Kermit,” she says. “I told [Wiley], quality has to be our top priority, because incompetent doctors hang out in rural areas.” Wiley, the three nurses agree, wasn’t much for listening. “He didn’t want us looking at anything or making comments about anything,” Mitchell says. “He was the administrator, and that was how it was.”
Four months after he started, Wiley hired Dr. Rolando Arafiles, a Filipino family-practice doctor he’d met at the hospital in Crane. Arafiles and his wife bought a house in Kermit. They threw themselves into the town’s social life. Arafiles played golf with the county sheriff. Wiley, who wanted his doctors to be part of the community, was thrilled—so much so that when the nurses started to question Arafiles’ treatment of patients, the administrator tried to quash their complaints. When Mitchell, Galle and Warren finally sent damning evidence to state regulators, Wiley and two of Winkler County’s leading citizens took decisive action: They launched an attack on the nurses.
When Arafiles started working at Winkler Memorial in April 2008, he was assigned to the attached Rural Health Clinic. Naomi Warren, who had worked in the clinic for more than 10 years, says Arafiles was initially well-liked. He smiled a lot, patted people on the back, took an interest in their lives. “From almost the beginning, though, it was clear that his care was questionable,” Warren says. “He isolated himself. He had his own nurse. He gave care in the back of the clinic, so it was not obvious to all of us what kind of care he was giving.”
Not at first, anyway. Warren began to notice Arafiles’ patients leaving the clinic with “little bottles of various solutions or samples of drinks. Many patients told me they had been given samples of solutions to drink that he said would cure many ailments.”
As he would later admit in court, Arafiles was giving patients samples of dietary supplements, often in place of conventional medicine. He sold these supplements on his website, health2fit.net. According to some accounts, he also sold them out of his office in the clinic. Patient reviews on the doctor-review site Vitals.com complain about Arafiles’ pitching non-FDA-approved supplements that patients could only get from him. One commenter, “Judy,” writes that when she came to Winkler Memorial with a chronic complaint, Arafiles offered her a “magic pill.”
“I asked if I could read up on it in any pamphlets or studies,” Judy writes, “and he said it’s new so there isn’t any studies or pamphlets that show it actually works.” She says she asked if she could order the magic pill over the phone, and, “He says, ‘Oh no, you can’t get it at local stores … but for $78.99 you can have a two month starter pack to try it out, and then it will be time for your next appointment with me.’”
The supplement was called Zrii, made of fruit juice and advertised as “based on the ancient wisdom of the Ayurveda” and sold by a multilevel marketing system. At the same time he was working in the hospital, Arafiles was holding seminars at the Kermit Pizza Hut and the Methodist Church, signing people up as Zrii distributors.
By July, Warren noticed that the new doctor had begun to “change medicines on patients who had been on thyroid meds for many years and were stable.” Worse, he was not rechecking them to make sure the new medications were working. Arafiles, as the Texas Medical Board would later find, also prescribed powerful thyroid-stimulating drugs to patients who came into the hospital with common maladies like stomach pains or sinus infections. Putting a healthy person on thyroid stimulants is dangerous, Warren says. The drugs can cause hyperthyroidism in healthy patients—unchecked, that can lead to permanent organ damage and death.
Now alarmed, Warren asked Arafiles to explain his treatments. “He attempted to get me to do the same thing,” she says. “He explained to me at length that the thyroid numbers in a lab aren’t important—that’s not what you look for. You look for obesity, extra fat behind the arm, fatigue, and that’s all you need to know.”
Warren had never heard of such a diagnostic practice, and she couldn’t find any support for it in the medical literature. She told Arafiles she wouldn’t prescribe thyroid stimulants on the basis of patients’ appearance without medical data to support it. So Arafiles gave her data that, she says, shocked her even more. “He brought two paperback books that were obviously alternative medicine. [The author] was a person—I’m not sure if he was a doctor, but he had studied corpses and had determined that these symptoms showed the need for thyroid.”
By September 2008, five months after Arafiles came to Kermit, the nurses in charge of Winkler Memorial’s quality control were getting strange reports of another serious problem with the doctor’s work. He was performing unconventional surgeries. He wasn’t a surgeon, and the hospital wasn’t supposed to perform surgeries.
There was, for starters, the patient who came in with a compound fracture on his thumb. According to the Medical Board, Arafiles “sutured part of a rubber tip removed from suture kit scissors to the wound on [the patient’s] right thumb.”
Then there was the woman who dropped a frozen turkey on her foot. Arafiles hammered a needle in to serve as a post to “stabilize the bone.”
And there was the 73-year-old diabetic who came in with a gash on his hand that would require a “full thickness skin graft.” In the past, such patients would be sent to Odessa. Arafiles took care of it himself. He cut a strip out of the man’s abdomen and did the graft. One week later, according to a nurse who worked under Arafiles, it had failed: “There was no blood supply. It was black, like charcoal.”
As Anne Mitchell read through the charts the floor nurses were leaving on her desk, she was dumbfounded. The things Arafiles was doing, she says, “just didn’t make sense. If we were in a Third World country and had no access to health care, I could understand. But we were 35 miles away from excellent medical care in Odessa. There’s no excuse for sticking a needle in someone’s toe, or putting a skin graft on a diabetic man.”
Because Arafiles wasn’t checking up on the patients, it fell to the nurses to catch his mistakes. According to Debby Eggers, a clinical nurse who sometimes worked with the doctor, Arafiles rarely even looked at the patient charts. “He didn’t even open up his charts to clarify age or the patient’s name,” Eggers says. “He never looked at anything. He told me that he was glad I worked on his side because I was his eyes, because he never looks at anything, he only signs his name. That’s word for word.”
As evidence of Arafiles’ bizarre doctoring mounted, Winkler Memorial’s old hands—nurses Warren, Mitchell and Galle—started trying to get the hospital administrator to rein him in. When she first went to Stan Wiley in September 2008 to express her concerns, Naomi Warren says she didn’t want Arafiles fired or reprimanded. She just wanted him to follow the rules. She assumed that Wiley, with his interest in keeping the hospital from being sued, would feel the same way.
“I told him that Arafiles was giving off-label, non-FDA-approved medicine, and that he was going to hurt people. I said, at least if you’re going to let him do this, you might as well have the patients sign a waiver so they know what they’re getting.”
The waiver, she says, was not a serious suggestion. “I was trying to get him to realize how ridiculous it was,” she says. Wiley thought it was a great idea. He asked Warren to write up a waiver form for Arafiles.
Anne Mitchell was also telling Wiley about the strange reports crossing her desk. In September, Wiley asked her to write a letter to Arafiles, reminding him about hospital policies. The policies cited in the letter were head-slappingly obvious. For example, “medications used by physicians and allied health care must have been approved by the regulating agency i.e. FDA, and have the necessary documentation indicating dose benefits, possible adverse effects, drug interactions, etc.”
Wiley declined to take any further measures. So Mitchell, Warren and Galle, the quality-control chief, took their complaints to the hospital board. At one meeting, Galle talked about the cases—including the failed skin graft and the needle-reinforced toe—that she was planning to send out for external review. As she spoke, she says, Wiley sat next to Arafiles with his arm over the doctor’s shoulder. “Arafiles looked like a little scolded schoolboy,” she says. “He said, ‘I didn’t know I couldn’t do those things.’”
At that point, Galle says, Wiley interrupted her presentation. The board, he said, would come back later to the complaints about Arafiles “when they had more information.”
“Mr. Wiley patted Arafiles on the back,” Warren recalls. “He said, ‘That’s OK, big guy. That’s OK.’”
Neither Wiley nor Bill Beckham, the president of the hospital board, was happy with the nurses. They seemed especially put out with the outspoken Mitchell. After a meeting in December 2008, Mitchell says, Beckham, a scion of one of Kermit’s oil-rich clans, told her that “everyone in the community liked Arafiles, and the only problems he was hearing from anyone were coming from me.”
Why were Wiley and Beckham protecting Arafiles? Wiley would later testify that Arafiles was a stellar employee, unfairly maligned. The nurses say Wiley had come to Kermit talking about how he was going to make the hospital money, and Arafiles was helping him do that—that the doctor was ordering lots of expensive, unnecessary tests and admitting patients to the hospital whether or not they needed to be there. When one man came in with an earache, Naomi Warren recalls, Arafiles ordered close to $1,000 in lab tests. “Arafiles never sent that man the lab results,” she says. “And he never looked at his ear.” The Texas Medical Board would later cite three instances in which Arafiles did “unnecessary genitourinary exams” on women who had come in with sinus or thyroid complaints.
As Mitchell continued to speak out about Arafiles’ treatments, Wiley allegedly tried to get rid of her behind the scenes. In addition to nursing, Mitchell worked part-time as the county Homeland Security director. In late 2008, Wiley tried to convince her boss there, County Judge Bonnie Leck, to take her on full-time. Leck declined.
At one point, the nurses thought they’d achieved a minor victory. Wiley set a meeting that was supposed to make clear for everyone—meaning Arafiles—what care was and wasn’t acceptable. But Wiley cancelled the meeting without explanation. Naomi Warren says she lost hope. “They beat me down,” she says. “I realized they were on a path they didn’t intend to get off of.” She quit in February 2009, 10 months after Arafiles was hired. According to another board member, when Beckham, the board president, learned she had quit, he said, “Well, if she doesn’t like Arafiles, let her go.”
When Warren took a job down the road in Monahans, more than 600 of her loyal patients chose to drive the extra 25 miles to Monahans to see her, resulting in revenue losses for Winkler Memorial. Her departure was part of a larger exodus of hospital and clinic personnel shocked by
rafiles and the ho
pital’s handling of him. Dr. Khoa Pham, the hospital’s chief of staff, had been fighting with Wiley about Arafiles and left in January 2009 as his contract expired. A few months later, Debby Eggers, the nurse who worked under Arafiles, and Corina Chavez, the clinic manager, quit to join Warren in Monahans.
Eggers says she left because “I couldn’t control Dr. Arafiles. And I couldn’t sleep at night wondering, what if I didn’t catch one of his mistakes?”
Mitchell and Galle were the only critical voices left in the hospital. In February 2009, they decided to report Arafiles to the Texas Medical Board. “We figured we’d tell the licensing body what was happening,” Mitchell says, “and let them decide what to do.”
This was a last resort. While the Bureau of Nurses Examiners requires that nurses take action when patients are being endangered, Winkler Memorial’s administration had issued different instructions. In a meeting in December 2008, Wiley had forbidden any reporting about doctors without his permission. The board changed the hospital bylaws to reflect the new policy.
Meanwhile, Naomi Warren was still troubled by what she’d seen at Winkler Memorial. She was working on her own letter to the Medical Board. She was also talking with Mitchell and Galle. In one of those conversations, Mitchell told Warren that she was worried about the complaint she was about to make to the Medical Board. Mitchell said she thought it was going to get her fired.
“I said, Anne, they can’t fire you,” Warren recalls. “They’ll never know we did it.”
In April 2009, the two met and compared notes. Their letters cited five patient charts each that the nurses felt were indicative of the problems the Medical Board needed to examine. The letters went out in the same envelope. Mitchell insisted on taking some security precautions. They mailed the complaint from Odessa, Warren says, “so it wouldn’t go through the Kermit mail.”
“I was a little bit put out with Anne,” Warren recalls, “because I thought, why are you being so cautious, why are you so upset and worried about your job?
“But I should have realized, I’m leaving—I don’t have to face the scrutiny of Winkler County and the officials there. I understand now. She had a much better handle on the kinds of people we were dealing with.”
Wiley and Arafiles had powerful allies—as powerful as it gets in Kermit. Two other men frequently attended hospital board meetings in which complaints were lodged against the doctor, though they didn’t work for the hospital. One was the county sheriff, Robert Roberts.

Roberts personified the phrase “West Texas sheriff,” with a big gut and a big voice. Roberts was good friends with Beckham, head of the hospital board, and Arafiles, whom he credited with saving his life during a heart attack in 2008. The sheriff and his wife signed on as Zrii distributors for Arafiles.
Rounding out the fivesome was Scott Tidwell, Arafiles’ and Roberts’ personal attorney. He had moved to Kermit in 2008 after being convicted of running a prostitution ring out of the Healing Touch massage parlor in Odessa. The sheriff had convinced Tidwell to run for Winkler County attorney, and helped him get elected.
In May 2009, Arafiles received notice from the Texas Medical Board that he was under investigation. As he later testified, the doctor went to Sheriff Roberts and asked him to find out who had reported him. Roberts got a warrant to seize Anne Mitchell and Vickilyn Galle’s computers. He found a copy of their letter of complaint on Galle’s hard drive. Two weeks later, Wiley called the nurses into the hospital boardroom, one at a time, and fired them.
“He looked at me and said, Vickilyn, your services are no longer required,” Galle recalls. “That was it. There was no explanation. I just signed the paperwork and left. His secretary told me that usually she was supposed to escort people out. But since I’d worked there for a while, she’d let me leave on my own.”
Ten days later, County Attorney Tidwell convened a grand jury to indict the nurses for misuse of official information, a felony that carries a possible $10,000 fine and a 10-year jail sentence.
“I was stunned,” Mitchell says. “I couldn’t believe they got an indictment against us, because we’d done absolutely nothing wrong.”
The case sent shockwaves through the nursing world. “If a nurse can get criminally indicted for reporting unsafe care to a licensing board,” says Jim Willman, head counsel for the Texas Nurses Association, “it’s going to have a chilling effect on their ability to report anywhere. The primary role of nurses is to advocate for their patients. They’re the health care provider with the patient the majority of the time. If the nurse isn’t there to speak up for the patient, the patients are going to be harmed.”
The association raised $47,000 for Mitchell’s and Galle’s legal defense fund. The money came from nearly 700 nurses and doctors in 44 states. The first donation was a personal check for $500 from a nurse in New York.
The nurses found the case so unbelievable partly because Mitchell and Galle were obligated to report unsafe care. “If something serious had happened to one of the patients,” says John Cook IV, Mitchell’s lawyer, “the state would have come in and they would have asked Anne Mitchell, ‘Why didn’t you report any of this? You’re the compliance officer. This is your job.’ At the very least, she could have lost her license.”
Tidwell apparently realized his case was weak. In July, he offered to drop charges if Mitchell and Galle would pay a small fine, do probation and—according to Mitchell—write a letter of apology to Arafiles and the hospital. They refused.
“They dragged us through all this,” Mitchell says. “We deserved our day in court.”
Only Mitchell would get that day in court. A week before the trial in February 2010, Tidwell dropped charges against Galle. Before the jury, the county attorney argued that Arafiles had been the victim of “a consistent pattern of harassment” by Mitchell. He conceded that nurses have a duty to report questionable care—but only if they’re doing it in good faith. Mitchell, he said, “was on a personal vendetta [against Arafiles] from day one.”

The case against Mitchell, he said, “is about one thing. It’s about a public servant that let personal animosity drive her decisions. That’s all it’s about, very simple.”
Cook, Mitchell’s lawyer, stood up. “Shame on them,” he said, pointing at Roberts, Wiley and Tidwell. “Shame on them for abusing their public trust. Shame on them for using the powers entrusted to them by us for their own personal gains and wishes. Shame on them for seeking to destroy professionals who for more than 20 years gave them their labors, their hearts and their soul. Shame on them for not having the honor to admit their mistakes. Shame on them for subjecting all Texans to ridicule by their Boss Hogg mentality.”
The jury took less than an hour to acquit Mitchell.
In June 2010, the Texas Medical Board filed a formal complaint against Arafiles, citing, along with his alleged medical infractions, his “unprofessional behavior” in getting the nurses indicted. On Oct. 4, 2010, Stan Wiley left his keys and a letter of resignation on his desk and slipped out of the hospital, never to return.
Read the transcript of Anne Mitchell’s trial.
I met Mitchell and Galle in January in the Winkler County Community Center, a squat, brick building across the street from the old courthouse. In the year since their trial, they have been feted as symbols of courage in nursing. They have received national nursing awards and are frequent speakers at nursing conventions. In August 2010, they won a $750,000 settlement from the county. In response to what happened in Winkler, the Texas Legislature is considering a bill, filed by Republican state Sen. Jane Nelson of Flower Mound, that would make it illegal to retaliate against a nurse for reporting anyone to a state licensing board. On March 1, Mitchell went to Austin to testify in support of the bill.
Despite being famous in the nursing world, Mitchell and Galle still can’t get jobs. Mitchell has applied for four medical jobs in West Texas, including one as a clinic receptionist. She hasn’t gotten any of them. She still works part-time as the county’s Homeland Security director.
“They ruined my career,” Mitchell says. “They ruined her career. I mean, where are we going to go? We both have lives here.”
Being known as a whistleblower, she says, doesn’t help. “They’re all patting you on the back, they’re all giving you accolades. No one wants to hire you. Hospitals think it’s great that oversight happens—they’re happy to implement changes from other places. But no one wants it coming from their facility. No one wants anyone looking at their doctors.”
As she talked about what happened, Mitchell alternated between bitterness and sadness. Galle, who is involuntarily retired at age 55, was more resigned. “I loved my job,” she says. “I thought I was going to work until I retired, then work part-time in the clinic. I guess that didn’t work out.”
I asked what she thought would happen to Arafiles. “Oh,” she says, “he’s a charismatic man. There are plenty of desperate hospitals in Texas. He’ll be fine.”
That is, if he doesn’t wind up in prison—along with his friends Stan Wiley, Sheriff Roberts and County Attorney Tidwell. In December 2010, David Glickler, a special prosecutor from the state attorney general’s office, convened a grand jury and indicted Arafiles on charges of felony retaliation and, in a karmic twist, misuse of official information. Three weeks later, he indicted Roberts and Tidwell for misuse of official information, official oppression and (for Wiley) felony retaliation.
The trial is set for June. None of the indicted men would speak to the Observer, saying that their attorneys had forbidden it.

In February, the Texas Medical Board released its final judgment on Arafiles. They let him keep his license, but put him on probation, required him to take continuing education classes and fined him $5,000. (A doctor in Odessa was given a $10,000 fine for yelling at a staff member in 2009.)
“This wasn’t really the outcome I was expecting,” Mitchell says. “I could have had a verbal confrontation with him, and he would have been more strongly reprimanded. I really believe that they still feel that nurses are expendable.”
Arafiles is out on bail and back at work at Winkler Memorial, although the board has decided to let his contract—which expires in April—run out without renewing it.
Most of the current staff I interviewed at the hospital express anger with Mitchell and Galle, whom they blame for making Winkler Memorial look bad. Shortly after Arafiles’ arrest, the hospital’s director of nursing, Donna Paehl, sent a letter to the Winkler Post, Winkler’s online newspaper, arguing that Mitchell and Galle had made nurses’ lives more difficult. “We have found ourselves in the position of policing the Physician’s [sic] because we are under such scrutiny,” she wrote. “It is not a nursing function to police the physicians and we will no longer be doing this.” But “policing the physicians” is an essential nursing function.
The hospital’s new compliance officer, the one who replaced Mitchell, is Peggy Armstrong. When I asked her about Arafiles, she said, “He’s a great doctor. Great. You shouldn’t believe the bad press.”
I asked Armstrong where the bad press had come from. She rolled her eyes: “Oh, you know. Just a bunch of vindictive small-town people.”
Read Dr. Arafiles’ censure and reprimand from the New York Medical Board.
Contributing writer Saul Elbein lives and freelances in Austin.