When Bovines Goes Bad
On April 27, 2004, a Texas cow dropped dead while waiting to be ground into beef outside a Gonzalez-area slaughterhouse. The death provoked particular concern among consumer advocates because it happened less than four months after scientists confirmed the nation’s first case of Bovine Spongiform Encephalopathy (BSE, or Mad Cow Disease) in Washington State.
The culprit in this high-profile case was a dairy cow born in Canada and fed with Canadian feed. Intensifying concerns was the fact that the USDA, of all agencies, had recently allowed 7 million pounds of Canadian beef to cross the border (under special permits that it forgot to make public). Making this scenario even more problematic was the recollection that many years ago a load of Canadian feed had accidentally made its way into American feed, satiating any number of cows capable of holding BSE in incubation for years. In light of the facts that BSE is caused by tainted feed and can manifest itself as Creutzfeldt-Jakob disease (CJD) in humans (thereby turning the brain into a sponge before inflicting death), anyone with a sliver of common sense would insist that—at the very least—the dead Texas cow be tested for BSE.
But in Texas, a country—oops, make that a state—where supporting “antievolution” gets you elected to school boards, common sense is at a dire premium. Rational deliberation on matters scientific is systematically undermined by a set of priorities that supports the beef industry at the expense of responsible public health policy. While one might wish to dismiss our evangelicals as nutso anti-enlightenment crusaders, their zealous efforts to subvert sound science with “Intelligent Design Theory” has led Holt, Rinehart, and Winston, for one, to have its backbone removed and publish ideologically tainted textbooks unconcerned with hard science.
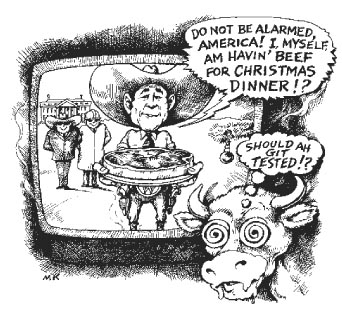
Relax, I’m not about to blame a publishing company for Mad Cow Disease. But the conspiratorially minded might ponder the connection between beef and fundamentalism with some justification. How else could we the Texas people possibly accept the USDA’s decision NOT to test that dead Texas cow and then turn around and declare with the utmost confidence, “We don’t have a new BSE case”? How else, were it not for plain old scientific ignorance, could we abide by our Bumbler-in-Chief’s April 2004 claim that “It’s in our interest that live beef [sic] be moving back and forth [from Canada]”?
How the Cows Turned Mad provides the hard science required to understand the genuine risk that Mad Cow Disease poses to anyone who chooses to spin the wheel and eat beef. While the book rarely deals with politics and policies, it’s a workman-like resource about Transmissible Spongiform Encephalopathies (TSE) that distills a wealth of scientific data into 200 pages of relatively accessible and soberly presented information about “The Disease,” its origins, and the myriad means of its contagion and transmissibility.
Keep in mind, though, the term relatively. While the proponents of “intelligent design” haven’t a chance of grasping the book’s intricate scientific explanations, even readers with a belief in genetics, protein synthesis, and nucleic acids will find many passages burdened with complexities that at least had me grasping for a student’s biology textbook (a real one) and getting a refresher on what really should be common scientific knowledge. While it seems an extreme measure to take in order to understand a trade book, might I trot out the cliché that knowledge is power. Might I also reiterate that those who already have power can hire people to manipulate that knowledge for them, leaving the rest of us to go about it on our own. We shouldn’t be lazy about this task because the beef industry and those who regulate it aren’t losing sleep over our health.
The Disease’s etiology began in the 1740s with the English quest to clothe the world in wool. The increase in sheep production naturally inspired greater attention to their health, leading one English farmer to take special note when a single sheep began “rubbing himself again Trees, Posts, & with such Fury as to pull off his Wool and tear away his Flesh.” The Disease, confirmed by strikingly similar reports in France and Germany, came to be called “scrapie.” Scientific knowledge being what it was before Mendel and Pasteur, some farmers attributed the strange behavior to “excessive copulation by rams.” Others who hypothesized the Disease’s infectious nature advised that the owner of a sick sheep simply slaughter the dizzy fur bag and feed it to the servants. Needless to say, the Enlightenment had its work cut out for it.
Maxime Schwartz, a professor at the Institute Pasteur in Paris, takes us from 1800 to 1920 with dutiful primers on Pasteur’s “three dimensional chemistry,” Mendelian genetics, and the chromosome theory of heredity. These pivotal scientific developments helped English scientists to hypothesize (correctly) that scrapie was infectious among sheep in natural conditions, most likely due to sheep eating grass upon which the placenta of another sheep had fallen. Not only was it infectious but, as scientists also discovered, scrapie could be positively identified by the presence of distinct vacuoles marking a sheep’s neurons like a bunch of spongy holes, an observation made possible with a basic microscope. This hypothesis and observation became integral starting points for the scientific community’s understanding of the disease.
Meanwhile, in an entirely unrelated context, an unknown German scientist named Hans Gerhard Creutzfeldt published in 1920 an obscure paper on “a Strange Focual Disease of the Central Nervous System” that he observed in a human patient he called “Berta E.” Remarking upon her rapidly diminishing coordination, as well as her rapid mental deterioration (“she thought herself demonically possessed”), Creutzfeldt found the loci of degeneration in “unusual brain lesions” that were odd enough to categorize Berta E.’s case as a new neurological disorder. When another German scientist named Alfons Maria Jakob published a paper describing several patients showing symptoms strikingly similar to Berta E.’s, a colleague of both men coined the term “Creutzfeldt-Jakob disease,” hoping way back in 1922 that the condition “will come to be thoroughly defined, in anatomical and clinical terms.”
Little could he have known the stealth the disease would use to elude such definition. Although nobody made the connection in the 1920s, we now know that scrapie and CJD were different adaptations of the same disease, a disease we now call Transmissible Spongiform Encephalopathy (TSE). Because CJD was so rare, Creutzfeldt’s and Jakob’s articles gathered dust for 30 years, leaving it to veterinarians to struggle helplessly, for example, with the scrapie epidemic that swept Scotland in 1937.
But again, in an entirely different context, new discoveries emerged to bring scientists closer to that ever-evasive definition. Watson and Crick demonstrated the structure of DNA in 1953, thus giving birth to the field that would ultimately explain the essential connection between scrapie and CJD and, later, BSE and CJD: molecular biology. With ideal communication, what scientists were coming to learn about proteins and nucleic acids in the lab might have had an immediate impact on animal pathologists’ understanding of scrapie’s infectious, transmissible, and hereditary qualities in the field. But, as Maxime writes, “A typical researcher has good knowledge about work in his own field, a little about related fields, and hardly any about more remote subjects.” And dizzy sheep up in the Highlands were nothing if not remote.
Were it not for the 1957 discovery of a Papua New Guinea community that made a culinary delicacy of each other’s brains, scientists may never have discovered the essential link between scrapie and CJD—a pivotal connection that would alert health officials to the epidemiological ramifications for humans when the cows began to go mad in the 1980s. Ritual cannibalism among the Fore people resulted in a disease called kuru. Turns out that kuru exhibited the same spongy cerebral lesions found in scrapie and CJD. With this suggestive link effectively established, the scientific community was finally piqued. After all, with people keeling over the way sheep were keeling over, the stakes were raised, money made available, prizes to be won.
Concerns focused on contagion and transmissibility. First, there was the question of how the disease spread—was it infectious or hereditary? Second, could it be transferred from one species to another? The regrettable answer to the latter question was yes. Scientists successfully transmitted scrapie to mice and kuru to chimps. Whether or not transmission to humans was possible could only be hypothesized, of course, but answers here were tragically forthcoming. What about contagion? Well, here’s where that biology textbook came in handy. Long (and complicated) story short: TSE is both hereditary and infectious and the causative agent in both forms of infection is a protein called a prion.
The prion violated everything that a molecular biologist worshipped as sacred. “It is,” Maxime writes, “a furtive protein that can cross the intestinal barrier, insinuate itself into the nervous system, crawl up to the brain, and enter the neurons and destroy them.” But because it is a protein—and not a foreign virus—the body cannot produce the antibodies required to defend itself. Whereas all other proteins have a single unchanging structure, the prion can spontaneously mutate into different forms, thus affecting the disease’s incubation period and the type of lesions it makes upon the nervous system. It was, furthermore, an infectious agent that lacked nuclei, but could still “somehow” reproduce itself. And it could, as mentioned, be passed on hereditarily. “A whole body of dogma,” as a result of the prion, had to be brushed aside before scientists could continue to pursue a preventive solution or, at least, a temporary cure for TSE.
Fortunately, when the cows started going mad, the prion had been fully accepted as a ruthless, mercurial, and persistent agent that followed its own set of twisted values. We still don’t know how cows contracted the disease that has come to be known as BSE. But when the English cows got sick, and when their neurons revealed those spongy holes, scientists and health officials had a very good idea of what they were up against. And they knew immediately that humans were at risk. There was, after all, every reason for BSE, should it be transmitted to humans, to manifest itself as CJD. Which leaves Maxime to answer one final question: How could it get to humans?
Here’s where the story might start to feel familiar. Scientists published the first article on BSE in 1987. One year later they learned that it passed among cows through their feed—a meat and bone meal mixture manufactured from cow carcasses. In 1996, the strong suspicion that beef eaten from an infected cow could cause CJD became stronger when 10 Britons contracted a new variant of CJD (nvCJD) that showed properties remarkably similar to BSE. “[The] apparent fact that the BSE agent was the same as that of nvCJD,” writes Maxime, “led to the nearly inevitable conclusion that the latter human disease stemmed from the BSE epidemic, and more precisely from the consumption of meat or other products from contaminated cattle.” The terrifying causal link had been made.
So that’s the science behind Mad Cow Disease. The most disturbing aspect of it all, however, is one that Maxime only touches upon by way of conclusion: Now that we know what causes nvCJD, our most pressing task is to regulate it. The United States, for its part, has talked a big talk on this score, banning outright feed made with bone meal. But the failure to test that Texas cow back in April reminds us that science, while beautifully illuminating the nature of this horrific disease, is also, as Edward Abbey once said, “the whore of industry.” Until we the general public learn more about the disease through important books like Maxime’s, we’ll be the ones getting screwed.
Contributing writer James E. McWilliams lives in Austin. He remains a carnivore (barely).


